COMPOSITION OF BLOOD

Components of Blood - average adult has about 5 liters (about 5 qts):
1 -
Formed elements:
Red blood cells (or erythrocytes)
White blood cells (or leucocytes)
Platelets (or thrombocytes)
2 -
Plasma = water + dissolved solutes
Red blood cell, platelet, and white blood cell
Red Blood Cells (or erythrocytes):

1 - biconcave discs
2 - lack a nucleus & cannot reproduce (average lifespan = about 120 days)
3 - transport hemoglobin (each RBC has about 280 million hemoglobin molecules)
4 - Typical concentration is 4-6 million per cubic mm (or
hematocrit [packed cell volume] of about 42% for females & 45% for males)
5 - contain carbonic anhydrase (critical for transport of carbon dioxide)
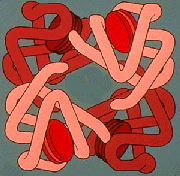
Hemoglobin 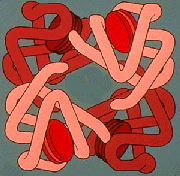

Composed of globin (made up of 4 highly folded polypeptide chains) +
4 heme groups (with iron)
each molecule can carry 4 molecules of oxygen
called oxyhemoglobin when carrying oxygen & called reduced hemoglobin when not carrying oxygen
can also combine with carbon dioxide & helps transport carbon dioxide from the tissues to the lungs
White blood cells (or leucocytes or leukocytes):
Have nuclei & do not contain hemoglobin
Typical concentration is 5,000 - 9,000 per cubic millimeter
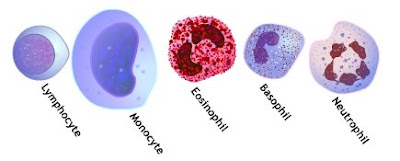
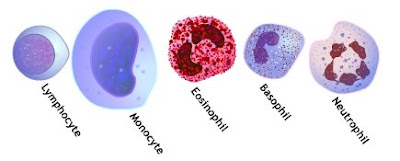 Types of WBCs:
Types of WBCs:
granular white blood cells include:
neutrophils (50 - 70% of WBCs)
eosinophils (1 - 4%)
basophils (less than 1%)
agranular (or non-granular) white blood cells include:
lymphocytes (25 - 40%)
monocytes (2 - 8%)
Granular white blood cells contains numerous granules in the cytoplasm, & their nuclei are lobed.
Agranular white blood cells have few or no granules in the cytoplasm & have a large spherical nucleus.
Granular white blood cells are produced in the bone marrow, while agranular white blood cells are produced in
lymph tissue, e.g.,
Lymph nodes (specialized dilations of lymphatic tissue which are supported within by a meshwork of connective tissue called reticulin fibers and are populated by dense aggregates of lymphocytes and macrophages).
The primary functions of the various white blood cells are:Neutrophils -
phagocytosis (bacteria & cellular debris); very important in inflammation
Eosinophils - help initiate and sustain inflammation and can activate T-cells (directly by serving as antigen-presenting cells and indirectly by secreting a variety of cytokines. Eosinophils can also kill bacteria by quickly releasing mitochondrial DNA and proteins (described below).
Eosinophils respond to diverse stimuli, including tissue injury, infections, allografts, allergens, and tumors. Eosinophils can also release a variety of cytokines, chemokines, lipid mediators, and neuromodulators. Eosinophils directly communicate with T cells and mast cells. Eosinophils activate T cells by serving as antigen-presenting cells.
Basophils - along with mast cells, play a role in inflammation and allergic responses
Release of histamine (that contributes to the 'symptoms' of allergies) by mast cells requires the production of antibodies (IgE) by B-cells andthat process is regulated, in part, by cytokines produced by basophils (Bischoff 2007).
Monocytes - phagocytosis (typically as macrophages in tissues of the liver, spleen, lungs, & lymph nodes) & also important antigen-presenting cells
Once distributed through the blood stream, monocytes enter other tissues of the body such as the liver (Kupffer cells), lungs (alveolar macrophages), skin (Langerhans cells), and central nervous system (microglia) (Gordon 2003).
Lymphocytes - immune response (including production of antibodies)
Eosinophils (in green with red nucleus) catapult their mitochondrial DNA out of the cell, forming tangled traps (red) that ensnare foreign bacteria.
Platelets (or
thrombocytes)
1 - formed in the bone marrow from cells called megakaryocytes
2 - have no nucleus, but can secrete a variety of substances & can also contract (because they contain actin & myosin)
3 - normal concentration in the blood is about 250,000 per cubic millimeter
4 - remain functional for about 7 - 10 days (after which they are removed from the blood by macrophages in the spleen & liver)
5- play an important role in
hemostasis (preventing blood loss)Plasma:1 - Water - serves as transport medium; carries heat
2 - Proteins
Albumins 60-80% of plasma proteins
most important in maintenance of osmotic balance
produced by liver
Globulins
alpha & beta
some are important for transport of materials through the blood (e.g., thyroid hormone &
iron)
some are clotting factors
produced by liver
gamma globulins are immunoglobulins (antibodies) produced by lymphocytes
Fibrinogen
important in clotting
produced by liver
3 - Inorganic constituents (1% of plasma) - e.g., sodium, chloride, potassium, & calcium
4 - Nutrients - glucose, amino acids, lipids & vitamins
5 - Waste products - e.g., nitrogenous wastes like urea
6 - Dissolved gases - oxygen & carbon dioxide
7 - Hormones